Mapping early signs of cardiac dysfunction in children using ultrasound
Children with dysfunction of the right heart chamber (ventricle), which pumps blood to the lungs, have lower tolerance to exercise and are at risk of sudden cardiac death in more severe cases. This dysfunction usually sets in progressively and detection at earlier stages is crucial to guiding therapies and interventions that improve symptoms and survival. New ultrasound techniques, make it easier detect and quantify the problem.
Assessing the right ventricular function has always been challenging with conventional ultrasound techniques. However, using the new high frame-rate ultrasound imaging techniques combined with speckle tracking (both developed at NTNU), we are now able to measure the energy that is lost in the blood. This is a promising new way of detecting ventricular dysfunction.
In the case of high blood pressure in the lungs (pulmonary hypertension), an early diagnosis is crucial to direct therapies, which can lower the resistances in the lung vessels and facilitate the function of the right ventricle, and reduce the risk of heart failure and sudden cardiac death. We have included 9 children, aged 5 months to 8 years of age, to study energetics and flow patterns within the right ventricle and pulmonary arteries, and compare these to controls.
Another particularly challenging group with regards to assessing cardiac function, is patients with single ventricle physiologies. This type of circulation refers to situations where one of the ventricles is inadequate to participate in pumping the blood to the body or to the lungs. The entire pumping function then falls on one ventricle instead if two. This type of circulation depends heavily on good ventricular performance and a large number of these patients experience ventricular dysfunction during adulthood. This can even go as far as requiring heart transplant, although this has limited success. Recognising dysfunction before patients develop symptoms is very important as it can offer a window of opportunity to intervene, either with medication or surgery, to improve cardiac function. Flow dynamics and energetics are particularly interesting to study in these patients as they may reflect dysfunction earlier than conventional echocardiographic parameters. We have included 21 patients, aged 4 to 9 years old, with this condition and will shortly start studying their intracardiac flow characteristics, including energy loss.
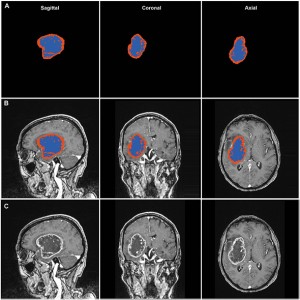
Studying these flow phenomena by imaging requires high frame rates because the blood moves much faster than the heart muscle (myocardium), with important phenomena occurring in short times intervals. Recent advances in imaging technologies have given us access to characterising the speed and volume of the blood flow (blood flow velocities) as never before. Blood speckle tracking, which is the technique our group is working with, combines ultra-high frame rate imaging (in the KHz range – see figure below), and tracking of speckles within the blood pool. From there, the velocities of these speckles can be measured without the use of contrast agents or the need for mathematical assumptions. These velocities measurements enable us to, amongst other things, to assess the energy loss.
Previously, we have studied cardiac flow dynamics in repaired tetralogy of Fallot, a condition where there is narrowing between the right ventricle and the lung artery requiring surgery. After the surgical repair, there is a necessary incompetence of the lung valve, which causes gradual dilatation and dysfunction of the right ventricle. A total of 57 children aged two weeks to 10 years were included. Of this group, 21 had repaired tetralogy of Fallot and 11 had an atrial septal defect (ASD) which is a hole between the upper chambers of the heart also causing right ventricular dilatation. In the latter 2 group, we found significantly higher diastolic energy loss compared to normal controls. Inefficiencies within the heart has long been suspected but to demonstrate these using non-invasive, ultrasound imaging is very promising in allowing early detection of flow inefficiencies at an earlier stage where interventions might be more beneficial.
Now that these techniques are available more widely, there are many challenges for our community to better understand, validate and compare flow parameters in normal and abnormal hearts. More technical improvements are needed with regard to developing 3D techniques, where NTNU is making great leaps.
How these new insights alter our management to improve our patients’ outcomes is to be seen as our community continues to explore these new imaging technologies.
Wadi Mawad
- Wadi Mawad#molongui-disabled-link